Prostate cancer screening with a prostate-specific antigen (PSA) blood test should follow a “shared decision-making” approach. The goal of shared-decision making includes a combination of the patient’s wishes and desires with guideline recommendations (focusing on benefits and harms), as explained by the physician, in order to make a PSA screening plan that is optimal for each man. Most urologists in the United States rely on the American Urological Association (AUA) guidelines to counsel patients for PSA screening. Generally, these guidelines suggest that:
- For men between 55 and 69 years of age, the decision to undergo PSA screening involves weighing the benefits of reducing the rate of metastatic (i.e., advanced) prostate cancer and prevention of prostate cancer death against the known potential harms associated with screening and treatment
- Routine PSA screening is not recommended for men aged 70+ years of age or any man with less than a 10 to 15-year life expectancy
When deciding on whether PSA screening is appropriate, patients, their physicians, and health care decision-makers including those who write guidelines must consider the risks and benefits. The rationale for restricting PSA screening to men under the age of 70 is driven by evidence that suggests that finding asymptomatic prostate cancers using PSA screening is only beneficial in men who are going to live at least 10 more years. This is because of the expected rate of growth/spread of these tumors. It is unlikely that an asymptomatic tumor found based on PSA screening will harm a man in less than 10 years. Indeed, the studies of prostate cancer screening have not shown improvements in mortality with screening for men older than 70 years of age. However, these men still have the risk of harm from follow-up testing including biopsies after PSA screen and overdiagnosis, with harm related to the treatment of cancers that never would have caused harm. Thus, it is believed that the harms of screening may outweigh the benefits in an older population. However, the AUA guidelines do note that men age 70+ years who are in excellent health may still benefit from prostate cancer screening.
It is important to note that large population-based studies have shown that men diagnosed at 75 years of age or older account for nearly half of the cases of metastatic (advanced) prostate cancer and just over half of the prostate cancer deaths, despite representing a quarter of the overall population. Furthermore, many men are living longer and are still healthy and active into their 70s and 80s, thus potentially benefiting from PSA screening for prostate cancer. Balancing these factors, it is important to understand which men may benefit from PSA screening and consider factors beyond just age.
Calculating a man’s life expectancy is one such way for patients and doctors to decide whether PSA screening may be appropriate. For men 70 years of age or older, it is important to understand life expectancy and what factors into these calculations to figure out the usefulness of PSA screening for prostate cancer. Studies have suggested that PSA screening occurs in up to 20% of men who have a life expectancy of fewer than 10 years. These patients have very little to gain from PSA screening (even if cancers are detected) but are at risk of the harms of screening.
The accompanying life expectancy calculator (designed by Hawken, SR et al.) assigns a point value of 1-5 for comorbidities (other medical conditions you may have) based on their impact on survival (Step 1). The total number of comorbidity “points” are then added up (Step 2) to classify each man into a comorbidity group: none (0 points), intermediate (1-4 points), and high (equal to or more than 5 points). The following table (Step 3) is then used to estimate life expectancy < 10 years (for which PSA screening for prostate cancer is less likely to be beneficial), accounting for race and comorbidity:
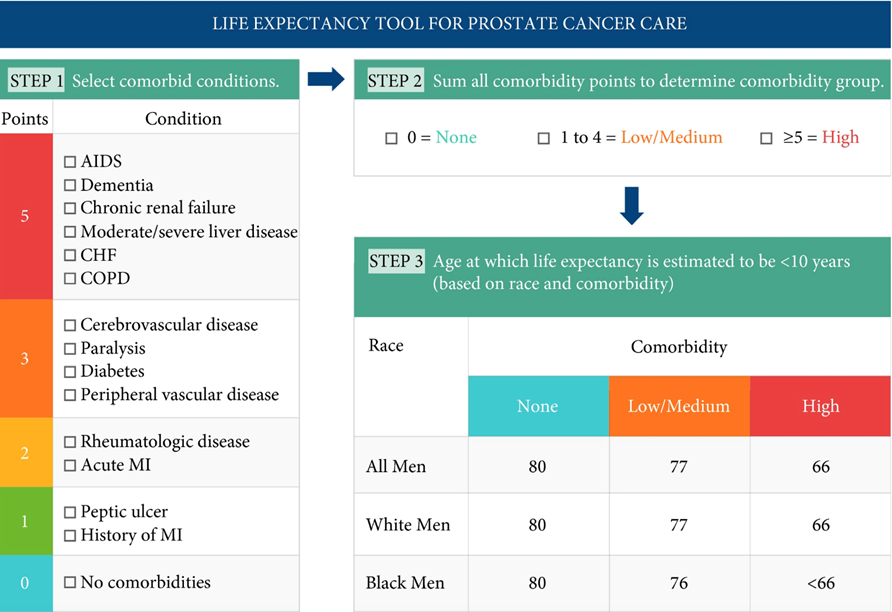
*Hawken SR et al. Calculating life expectancy to inform prostate cancer screening and treatment decisions. BJU Int 2017;120:9-11.
It is important to note that the majority of early (localized) prostate cancer does not cause symptoms such as a slow urinary stream, leakage of urine, or getting up at nighttime to urinate. As men age, the prostate gland continues to grow (also known as BPH: a benign, non-cancerous process), which is far more likely to cause these symptoms, also known as “lower urinary tract symptoms.” While this may still prompt a visit to your urologist, it should not be mistaken for signs of early prostate cancer, as this is more often than not related to accumulating birthdays.
If a PSA screening test is done and a decision is made to proceed with a prostate biopsy in men 70+ years of age, detection of prostate cancer does not necessarily mean that you will need treatment. For low-risk and even some intermediate-risk disease, active surveillance is likely a safe and reasonable management plan for your prostate cancer.
Life expectancy calculators, such as the above example, may help men understand how guideline recommendations relate to individual cancer diagnoses or screening options. Understanding the results from a life expectancy calendar can help to facilitate discussions around goals of care. It can also improve shared-decision making about PSA screening for prostate cancer in older men. Healthy senior men in particular should engage with their doctor in a shared decision-making fashion regarding the risks and benefits of PSA screening for prostate cancer.